
Listen to the audio version of this story:
According to the Canadian Psychological Association, about 15 per cent of Canadians will experience at least a mild case of Seasonal Affective Disorder (SAD) in their lifetime — not just the “winter blues” but a form of depression that spikes in the fall and winter.
During the colder months, people who experience SAD see a drop in motivation and energy levels, suffer from fatigue despite adequate sleep, and lose interest in activities they usually enjoy. Their interpersonal relationships sometimes suffer as well. For some, the symptoms may have already started to surface at this point in the year.
Diana Brecher, a clinical psychologist at Toronto Metropolitan University (TMU), said SAD’s effects can cause someone to behave like a hibernating bear. “You kind of collect all the food and go in your cave and sleep for the winter,” she said. In other words, your body dictates what it thinks you need.
Canadians are particularly susceptible to SAD since our geography means we get decreased sunlight during the lengthy winter months. However, there are several ways that people can try to prevent SAD from recurring or — at least — mitigate the worst of its effects.
There are no shortcuts, though: to a significant extent, managing SAD involves making certain lifestyle changes.
“The only way out is through,” said Brecher. “You have to regulate sleep, start getting as much natural daylight as you can, and start eating differently.”
For students especially, time and budgetary constraints will play a factor in which remedies to try, and how easy it is to try them.
Natural Sunlight
Combating SAD starts with getting plenty of exposure to light — the right kind, at the right time of day — and the cheapest source of light is free: the sun.

The idea is to get plenty of natural light exposure during the day, coupled with avoiding artificial light, such as screens, at night, said Dr. Richard Horner, professor of medicine and physiology at the University of Toronto (U of T) and Canada Research Chair in sleep and respiratory neurobiology.
“The reason why this is so good is because, in winter especially, that powerful light in the morning is like moving the hands of a watch… earlier in the day,” said Horner. “So by the time evening comes, that body clock is saying, ‘Okay, it’s nighttime,’ because it was so strongly influenced by lights in the mornings, people start to feel tired, and they go to bed, get a longer night’s sleep… wake up in the morning mood is improved.”
Students can soak up the benefits of natural light simply by keeping their blinds open through the day, removing any objects blocking light, and taking frequent walks outside. Walking to school or getting out in between classes is a good way to accomplish this.
“On a really crappy day, sit next to a window, go into halls with windows, go to the Student Learning Centre,” said Brecher. “There are places that are well-lit, and they will make a difference.”
Vitamin D
The best-known benefit of sunlight is its ability to boost the body’s vitamin D supply, which in turn encourages serotonin production, the chemical messenger that stabilizes mood. This vitamin is popularly thought to be useful in fighting SAD, but its role has been studied with mixed results.
While vitamin D deficiency is present in those with SAD and may be a risk factor for depressive symptoms, the U.S. National Center for Complementary and Integrative Health (NCCIH) states that experts are uncertain whether consuming foods rich in vitamin D such as fortified milk, cereal and salmon, or taking vitamin D supplements, can relieve SAD symptoms.
As SAD expert Shari Harding told HuffPost, seasonal depression is a complex disorder and its presence cannot be solely pinned to vitamin D deficiency when it is usually a combination of environmental factors, circumstances, and/or physiology.
Sleep Patterns
Often depressive moods and fatigue make the body think it needs more sleep. But oversleeping has been linked to a host of medical problems including weight problems and back pain. While napping is normal, Horner says, adequate nighttime sleep is still vital to a healthy circadian rhythm.
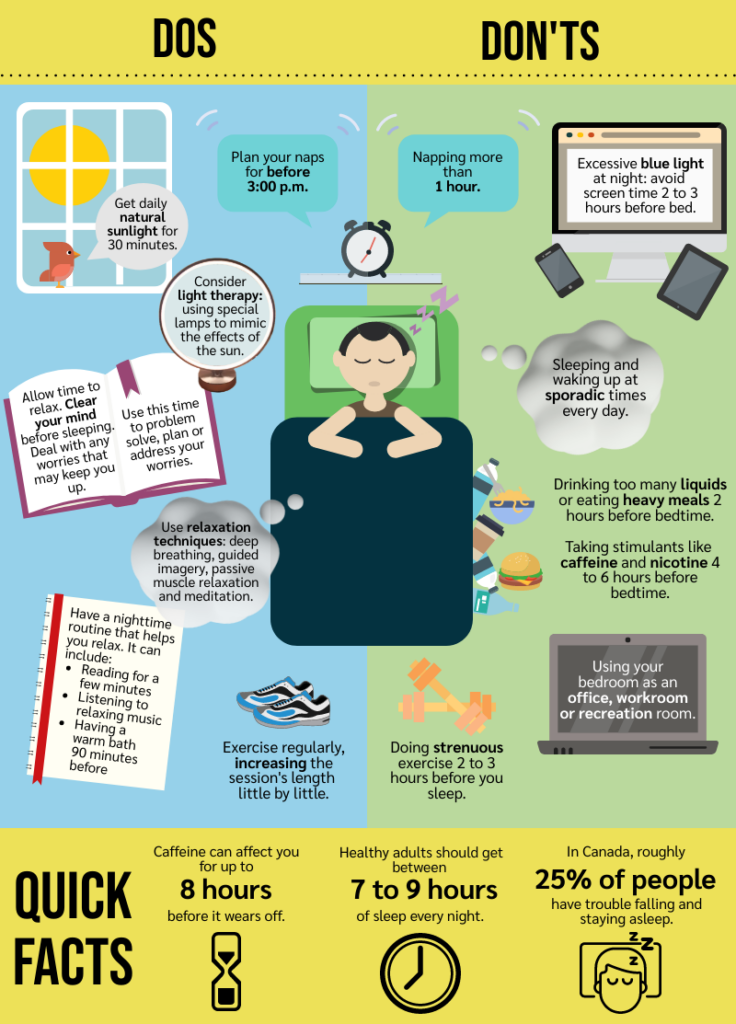
Horner says it’s easy to mismanage sleep, regardless of age, but most tips for better sleep are ones we often already know, including avoiding blue light and stimulants before bedtime.
Sources: The University Health Network, Sleep Foundation, Statistics Canada
The University Health Network’s (UHN) “Helpful Hints for Better Sleep” guide recommends simple ways to improve sleep such as exercising regularly, avoiding too many liquids or heavy meals two hours before bedtime, and timing naps for before 3:00 p.m. and keeping them under one hour.
Brecher recommends students consider downloading Doze, a free app for youth to help regularize sleeping patterns which was created by Dr. Colleen Carney, the director of the Sleep and Depression Laboratory at TMU, in conjunction with young adults.
Diet & Supplements
It’s common to crave foods that are high in fat, carbs, starch and sugar during times of stress because they provide immediate gratification. While they can create an initial spike in mood, the body burns through these foods quickly and then crashes, ultimately worsening a person’s mood.
One part of combatting this is avoiding copious, unrestricted consumption. Another is making sure to get enough nutrients and eat food that stabilizes and supports mood.
Individuals should maintain healthy levels of vitamin B12 (which helps the body convert protein and fat into energy) and omega-3 (which can easily travel through the brain cell membrane to interact with mood-related molecules). Choices include fish, poultry, and eggs for vitamin B12 maintenance; and flaxseeds, chia seeds and fatty fish like mackerel for sources of omega-3. Keep in mind these are not exhaustive lists, and various supplements are available as well.
Dark green leafy vegetables are also instrumental to combating SAD. They’re a good source of folate and magnesium which, research from The National Center for Biotechnology Information in the U.S. shows, are important in the prevention of depression. Seasonally-available options include collard greens, turnip greens, and spinach.
Fermented foods that nourish the gut, such as kimchi or plain yogurt, also help because gut bacteria produce about 95 per cent of the body’s serotonin.
Light Simulation or Light Therapy
Lifestyle changes aren’t enough for some people, which is why they may also turn to light therapy: sitting in front of SAD lamps or light boxes that are specifically designed to mimic the effects of the sun. These lights come in a range of sizes and brightness (and prices), and users generally sit in front of them for 30 to 60 minutes each morning.
Bayley Levy, a student at U of T in the final year of her Master of Science in Community Health program, experiences seasonal depression— and she’s already felt a dip in her mood and motivation this fall.

After inconsistent use of her light therapy goggles, she purchased a SAD lamp under the advice of both her psychiatrist and her therapist.
“I sit at my desk with my lamp every morning. I do work or I put on makeup. And some days I’ll notice that I feel a little more energized after the lamp, some days I don’t notice a difference,” said Levy. “But it’s one of those things that it’s over time. So I don’t want to judge it based on only a few weeks of usage.”
Pharmacological Treatments
SAD being a form of depression, coupled with evidence that it’s associated with a dysfunction in the brain’s serotonin systems, has guided researchers to look at pharmacological treatments such as antidepressants. These are usually recommended only in severe cases where SAD significantly impacts a person’s day-to-day functioning.
There are different categories of antidepressants, explains U of T’s Dr. Roger McIntyre, professor of psychiatry and pharmacology and head of the Mood Disorders Psychopharmacology unit at the UHN. These include selective serotonin reuptake inhibitors, selective norepinephrine reuptake inhibitors, and multimodal drugs that target several serotonin receptors in the brain.
“The drugs are similar, but they’re different in how they target different aspects of the brain,” said McIntyre, adding that most antidepressants take between four to six weeks to reach maximum effect. He says there is no evidence that one type of antidepressant is unequivocally superior to another because each person’s biology is different, so landing on the right prescription can take some trial and error.
Cognitive Behavioural Therapy
Research from the NCCIH shows that cognitive behavioural therapy (CBT) — a form of goal-oriented psychotherapy focused on changing habitual, maladaptive thoughts and reactions — can help to improve active symptoms of SAD while cultivating resilience against future episodes.
CBT sessions focus on immediate thoughts, moods, and feelings a person experiences with SAD, breaking them down into their constituent elements and making them more manageable. This strategy may also include practicing mindfulness and using various stress management techniques.
Brecher, who is certified in CBT, says it is sometimes more long-lasting than treatment with antidepressants since it helps an individual recondition their brain. However, people need to be patient with this approach. CBT is based on habit formation, Brecher says, so it may take two to three months of consistently repeating a behaviour.
Other forms of psychotherapy can help people manage SAD. As is the case with treating all kinds of depression, it takes some work with a therapist to figure out what combination of approaches will help a certain individual. Levy, the U of T student, has pursued a mix of Acceptance and Commitment Therapy and Dialectical Behavioral Therapy along with CBT.
You have to fight back, Brecher says. “The truth is you have to be conscious not to let [SAD] be this undertow that pulls you in.”
Listen to this week’s podcast episode: Singing the Winter Blues
News/Features Editor,On The Record, Fall 2022.
This article may have been created with the use of AI tools such as
News/Features Editor,On The Record, Fall 2022.


