
Listen to the audio version here:
Lynette George has a pile of two-week-old laundry taunting her to fold it.
She wants to do it. She knows she should do it. But she just can’t make herself do it. It’s a stagnating feeling that impacts nearly every aspect of the second-year journalism student’s life.
She’s pretty sure she has ADHD. But without a diagnosis, George is unable to access academic accommodations from Toronto Metropolitan University (TMU).
Last summer, George reached out to the university’s Centre of Student Development and Counselling (CSDC). She hoped to get a diagnosis and formal supports in place in time for the fall term.
After a few consultations with a doctor, she was put on the waitlist for a psychiatrist. She was told she would most likely meet the psychiatrist sometime in the fall — well into her academic semester.
“It’s kind of annoying because… it’s already impacted half of a semester,” she said.
READ MORE: More online therapy key to dealing with growing demands for mental health counselling
In early November — in response to concerns about long waitlists for counselling services — TMU held a referendum seeking more money from its students. The referendum asked them to consider paying nearly 10 times more than they currently do for health services.
Right now, students pay approximately $4 per semester. The new fee will charge students an additional $34.90 per semester, totalling around $39, starting next September.
On Nov. 4, the referendum passed by 571 votes. Of approximately 46,000 eligible voters, less than 4,000 voted: 2,218 for the increase and 1,647 against.
TMU’s chief responding officer Colleen Dempsey told OTR that the referendum did not require a minimum voter turnout to validate its results. So while only 8.5 per cent of students turned out to vote, 100 per cent of students must now pay the extra $34.90.
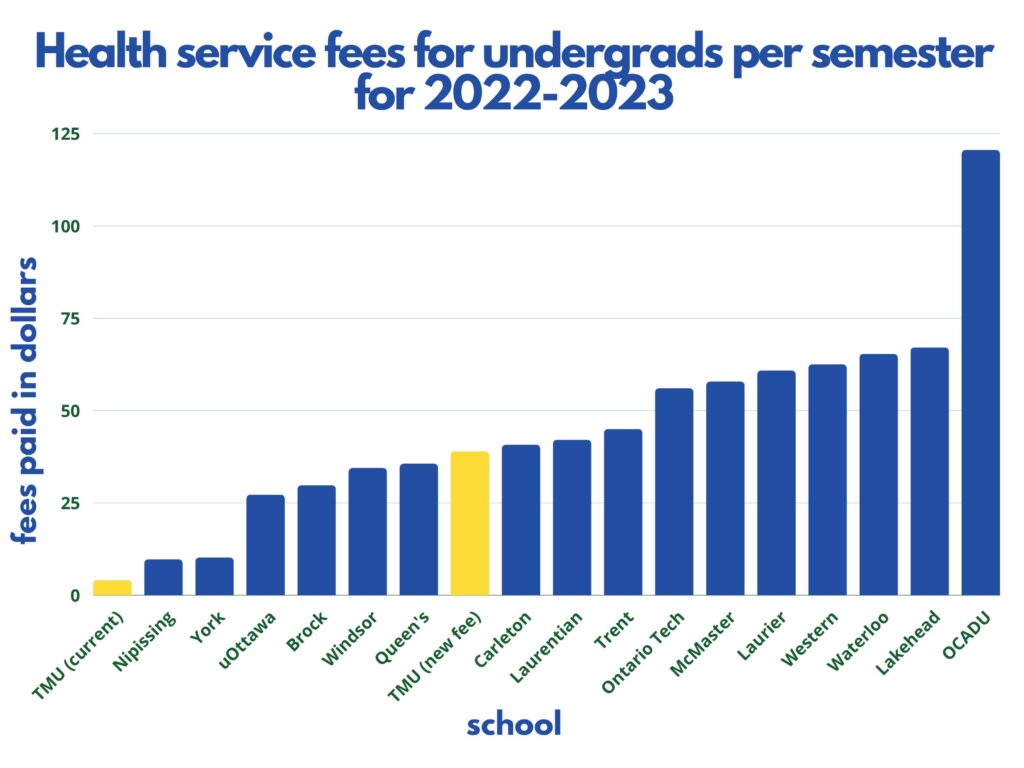
The additional fee will bring TMU to the middle of the pack when compared to what other post-secondary students are paying in health and wellbeing fees in Ontario.
But even the prospect of a fee hike didn’t sit right with some community members because of the lack of transparency around how exactly the university plans to implement proposed improvements.
With about 46,700 students, excluding continuing education students, the increase means the school — already receiving roughly $187,000 from the current levy — will receive nearly $1.7 million more each semester.
For years now, the university has said more funding will allow for improved wait times, but it’s not clear if it has. Students waited, on average, 14 weeks for a counselling appointment last year — an increase of more than 12 per cent from pre-pandemic wait times.
In 2016, the school announced that it would hire additional staff and implement online modules for students as a pre-emptive measure to counselling, or as a tool to be used alongside counselling.
Since November 2019, students have not had the choice to opt out of the wellness fee. On top of out-of-pocket expenses and long wait lists, fears of racial discrimination are some of the other barriers students may face when seeking care. Last year, On The Record reported that of the 21 counsellors at the CSDC, there were only three who identified as Black.
The COVID-19 pandemic has had a notable impact on student mental health, as well. In 2020, Statistics Canada found that 64 per cent of people aged 15-24 reported declining mental health. Job security, finances, and workload were among the top listed stressors in another Statistics Canada report that year.
A 2021 report by the Mental Health Commission of Canada found that flexibility, efficiency, and adaptability of service delivery were the top priorities for post-secondary schools wanting to enhance student supports post-pandemic.
READ MORE: Amid worsening mental health, students are anxious to return to in-person classes
Students require more mental health support than before. Almost 5,000 students accessed TMU’s medical services in the 2021-2022 academic year, according to a spokesperson for the health and wellbeing department.
A majority of student visits are mental health-related, making up approximately 68 per cent of the medical centre’s total visits that year. With about 3,400 students using the CSDC’s services, that is a 55 per cent increase from the roughly 2,200 students who used the services in 2019.
Asking students — many of whom are struggling — to once again pay more to improve services is one of a number of strategies to consider, but mental health expert and TMU associate professor Corinne Hart has her reservations about its potential impacts.
“[They] need to be able to say, this is what you’ll get for your dollars…” said Hart. “What will it actually provide? How many counsellors? How much full time staff before just saying, ‘We’re going to give you wellness?”
The university has said a chunk of the money will be used to support construction of an all-new student wellbeing centre on campus. In a phone call with OTR, president Lachemi said that a minimum of 25 per cent of the fee will be “dedicated to frontline support that will come online for students in the beginning of the fall 2023 semester.”
How exactly the rest of the funds will be dispersed remains unclear, though additional staff, access to virtual counselling, and a one-stop shop for all student healthcare needs are among the allocations listed by the school.
“What will it actually provide? How many counsellors? How much full time staff before just saying, ‘We’re going to give you wellness?”
CORINNE HART
The school says it has been consulting with students and staff regarding the referendum and other wellness initiatives since last February.
“We have heard repeatedly from students that they find it hard to find where certain services and support are located on campus and are often shuffled from one office to the other,” Lachemi said.
Another complication is the process of booking an appointment with the medical centre or CSDC online. There are no simple website booking tools, so students have to call the centre or write an email.
In an attempt to better understand how the university allocates existing funds to the TMU medical centre and CSDC, OTR filed an Access to Information and Privacy request asking for a breakdown of the total sum of money received and/or allocated by the school towards the medical centre and CSDC from 2019 to present. In response, the university said it has “no records in its custody and control.”
Regardless of the lack of clarity around services, students who have been able to access the centre’s care say it has been beneficial.
This fall, one of Alycia Wheeldon’s classmates died. In early October, the third-year performance production student and her classmates were given priority at the CSDC for one-on-one counselling sessions as a result of the sudden tragedy.
It was the first time she says she really learned about the services TMU offered. But Wheeldon says the priority queue jump “also means [the university is] admitting to the fact that there’s already long waits.”
“If we didn’t have a bit of a priority, we might be missed,” she said.
Wheeldon says she wouldn’t mind paying more for lower wait times — so long as those who can’t afford to pay extra have the opportunity to opt out.
But not being able to pay extra fees is one of the reasons students like George rely on the medical centre in the first place. If George, an international student, tried to seek out an ADHD diagnosis elsewhere, the charges would be in the $3,000 to $4,000 range.
“That’s not an option for me. I have no option but to wait five months,” she said.
Meanwhile, George is still on the waitlist to see a psychiatrist, but she says it doesn’t seem like she will be seeing one anytime soon. “I am hoping, maybe, by my third year … that something happens,” she said. “But I just don’t have expectations at this point.”
Hart says the issue with access to timely counselling and mental health services is complex because it is difficult to pinpoint who the onus is on to create effective change.
“The big question is what do universities owe students in terms of mental health support,”she said. “Universities are places where we are teaching people how to be citizens, and they need those supports to be citizens who are going to live in society.”
READ MORE: Are racialized youth being left behind in mental health research?
Reporter, On The Record, Fall 2022.

