
Some junior doctors in the United Kingdom say they are interested in moving to Canada in pursuit of better working conditions but physicians here suggest they might not find what they’re looking for.
In Canada and the U.K., medical practitioners share similar concerns about unfair compensation, the burden of paperwork and burnout due to lack of adequate support. It’s therefore unclear if British doctors coming to Canada will improve upon their situation – or solve Canada’s family doctor shortage.
“Our systems are all experiencing challenges that we only begin to understand once we live through them ourselves,” Zoe Tsai, a second-year medical student at the University of Ottawa and the vice president of advocacy at the Ontario Medical Students Association, said in a Zoom interview.
She said British junior doctors should speak to physicians already practicing in Canada first, to determine whether their needs will actually be met in Canada’s struggling system.

British doctors struggling
A 2023 report conducted by the British Medical Association revealed that 60 per cent of junior doctors in the U.K. reported low morale and a further 51 per cent described their desire to continue working in the NHS as “low.”
Junior doctors have taken strike action 10 times since their first in 2023, in an ongoing dispute over pay.
While the medical association expects more strikes for the remainder of the year to demand better compensation, some junior doctors say they aren’t willing to hang around and see it through.
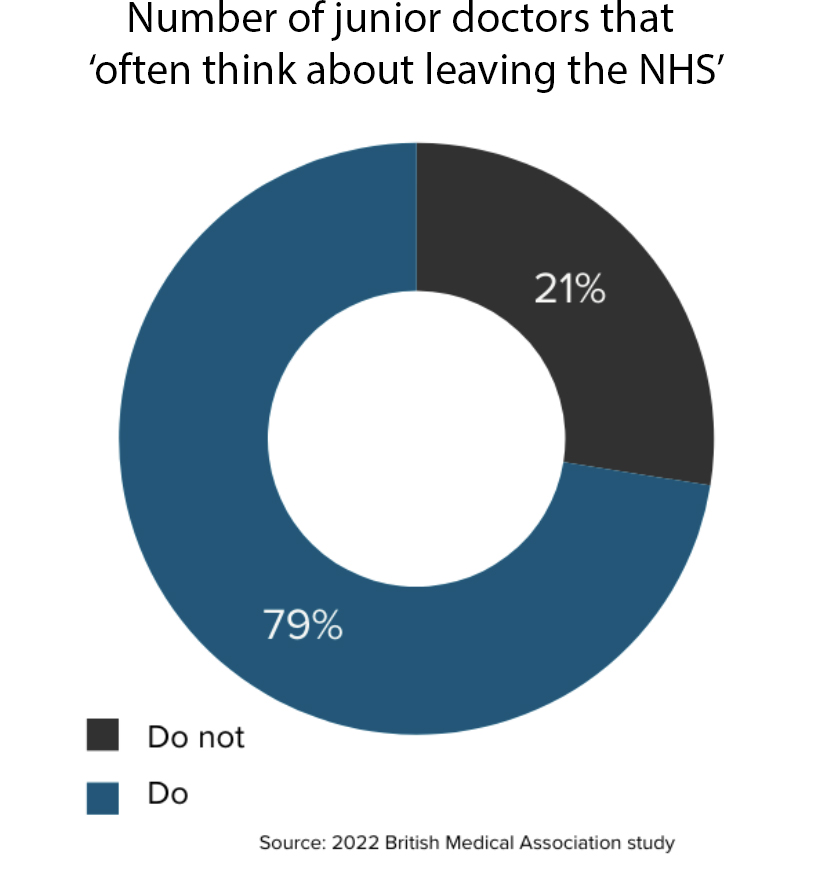
In two surveys conducted by the association, 79 per cent of participants said they often think about leaving the National Health Service and a third of respondents said they planned to work as a doctor abroad in the next 12 months. Australia and Canada are the most popular destinations.
The two countries approved 820 permanent residence applications for specialist physicians and general practitioners between 2020 and March of last year.
Simi Onanuga, a 24-year-old medical student in London, said the situation for doctors and nurses in the U.K. is “quite bleak.”
“I think the pay dispute and working conditions are making it very hard to work in the NHS as a doctor… But the way it’s being run with inadequate staffing and poor remuneration is driving people away,” she said in an online interview.
“Right now I’m very pessimistic about the future of the NHS… I have always considered moving away, and now I’m considering it even more. Australia is the classic one that people think of but I’d consider New Zealand and Canada too.”
Canadian doctors face challenges
Meanwhile, a recent survey found that 65 per cent of family physicians in Ontario are preparing to leave their practice or shorten their hours within the next five years. This follows a similar trend across the rest of the country, as physicians say they have grown tired without adequate support.
“It’s not a viable profession to stay in right now because of the workload and pay structure,” Dr. Montana Hackett, a first-year family medicine resident at Queen’s University, said in a Zoom interview.
Access to Family Doctors
chart by Daniyah YaqoobAn analysis by the Canadian Institute for Health Information found that Canada ranked last of 10 high-income countries in terms of access to healthcare. While the Commonwealth Fund average for access is 93 per cent, Canada lags behind at 86 per cent.
Still, Tsai, the Canadian medical student, said that Canada needs to increase the “supply” of doctors to meet the urgent needs of communities.
The Ontario College of Family Physicians found that about four million Ontarians – including one million Torontonians – will be without a family doctor by 2026. Among 10 high-income countries, Canada ranked last in how much of its population had access to family doctors.
“Adding to the crisis is a clear trend in medical students not choosing family medicine,” the college said in a press release.
But Hackett said it’s not enough to try and get more people into medicine. Instead, he said, retaining doctors who are already in the profession in Canada – by changing the workload and pay structure – should be the number one priority.
“If there aren’t substantial changes to how that works, then full-scope family medicine is not something I will do very long,” he said.
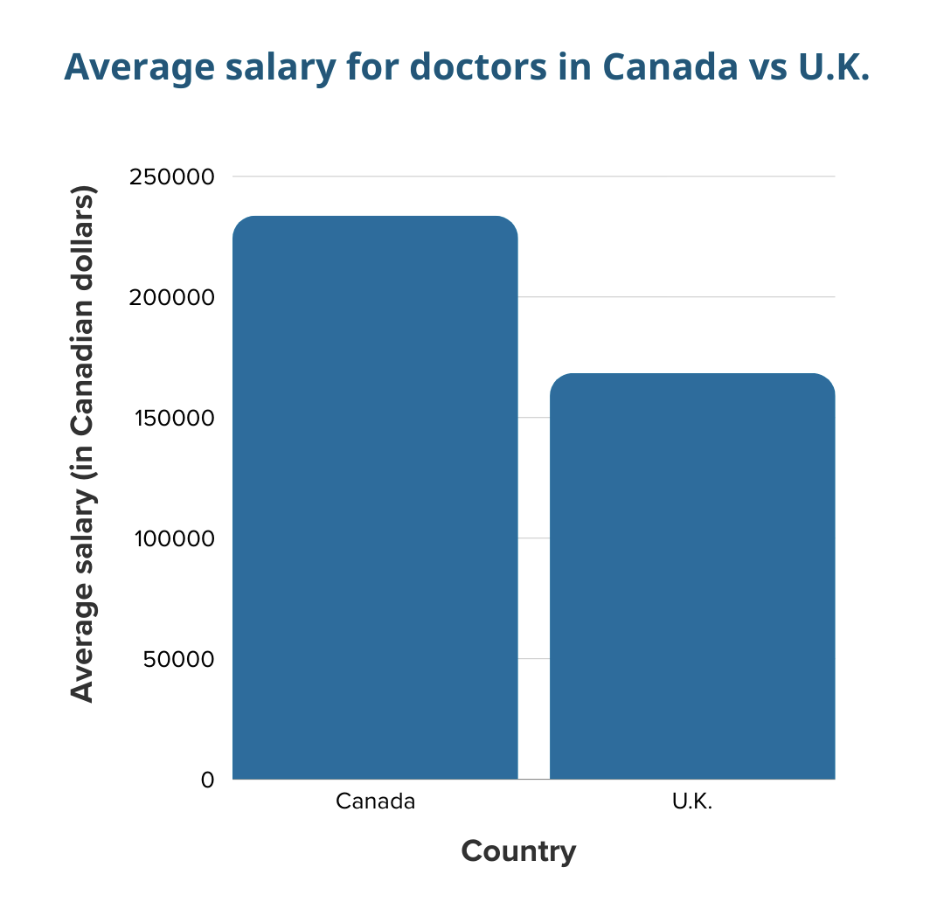
Right now, general practitioners in Canada earn an average of $233,726 compared to U.K. physicians, who make about $168,420.
While Canadian earnings are higher, Hackett pointed out that doctors often have to cover overhead and other costs associated with operating a business. British doctors coming to Canada for better conditions, Hackett warned, might struggle with the same situation.
Tsai said international medical graduates from England could also face challenges associated with obtaining medical certification to work in Canada – and that is an additional barrier to consider.
“An influx of junior doctors might temporarily strain resources dedicated to orientation, licensing, and integration into the Canadian healthcare system,” she added.
Canadian medical students have hope
Despite their concerns about practicing medicine in the existing system, Canadian medical students and recent graduates expressed hope that there is a better future in store.
Sam Alatorre, a final-year medical student at the University of Calgary, said family medicine is now being promoted and encouraged as a focus for students in medical schools.
“We’re riding this big momentum wave right now and I’m of the thinking that things are going to get better,” he said in a Zoom interview.
“We came into this field because we are problem-solvers, because we want to help people,” Tsai said. “When we see the crisis, we’re, if anything, inspired to help and do something about it.”
