
Listen to the whole story here:
A new national report from Statistics Canada highlights how some Canadians living with life-limiting illnesses are experiencing the current healthcare system through a voluntary crowdsourcing initiative.
The report, which reached out to 984 participants, found that older Canadians who participated in the study with advanced cancer were more likely to receive palliative care than any other group. In a portrait of participants, “over one-third (31 per cent) identified as persons living with a life-limiting illness in 2024, while nearly two-thirds (64 per cent) identified as unpaid caregivers.”
The World Health Organization (WHO) says palliative care is the type of holistic care that prioritizes not only physical needs, but also the patient’s emotional, social, and spiritual well-being. It can be delivered alongside active medical treatment.
A striking 80 per cent of those asked said that they had a very hard time finding some sort of care overnight or on weekends. According to the report, the most difficult services to access were pain and symptom management (36 per cent), referrals to specialists (35 per cent), and care coordination (31 per cent).
“I would suggest that accessing care overnight or on the weekends is difficult for everyone because of the reliance on family doctors and the fact that we have a shortage of them,” said Karen Soldatic, Canada Excellence Research Chair in health equity and community wellbeing. “The issue really is for people who have a lifelong condition or a life-limiting illness, is the fact that they often have to rely on ER specialists.”
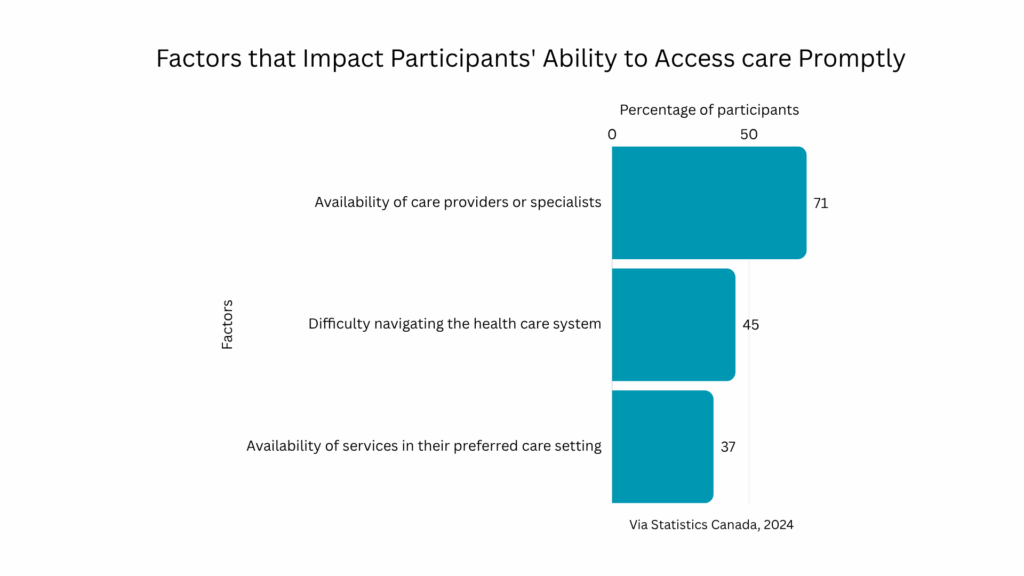
The three key factors reported as adversely affecting access to prompt health care were availability of healthcare providers or specialists (71 per cent), difficulty navigating the healthcare system (45 per cent) and a lack of services in their preferred care setting (37 per cent).
The study also spotlighted some major gaps in support for unpaid care providers, many of whom provide important assistance to loved ones with these conditions. Among these unpaid caregivers, 89 per cent said that their needs as caregivers had never been assessed formally.
“Because of the lack of services, the limitations around accessibility and inclusion, carers as a general population aren’t receiving the care and support that they need to care for themselves and also to care for the people that they’re responsible for providing care for,” said Soldatic
When it comes to the support they did receive, the results were mixed. Nearly half (49 per cent) of unpaid caregivers said they had at least partial access to services or assistance, though often not enough to fully meet their needs. By contrast, 39 per cent reported receiving no help at all.
“The medical professional needs training. There needs to be accessible clinics. [Professionals] need to be readily available and responsive. But what are the broader social structures in which people with what life-limiting illnesses and their primary carers actually need? What we call social protections to enable them to live well, a life that’s worth living,” said Soldatic.
CORRECTION: Statistics Canada used voluntary crowdsourced data to reflect participants’ experiences and advised us that this is not statistically representative of the entire Canadian population. OTR regrets the earlier writing that may have implied the data represented more than the participants’ experiences.
Otter.Ai was used to transcribe interview
